Introduction
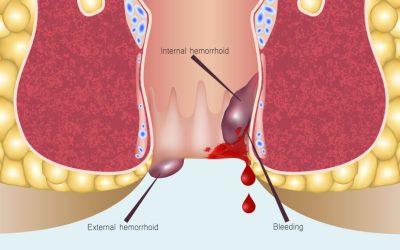
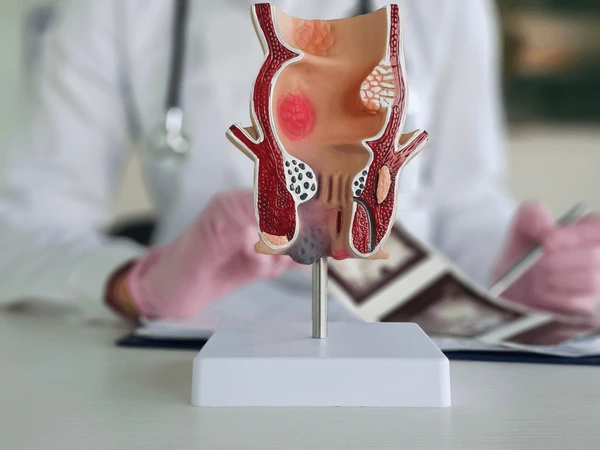
Hemorrhoids are a common and often uncomfortable condition affecting the veins around the rectum and anus. They can be internal—developing inside the rectum—or external, forming under the skin around the anus. Both types may cause itching, swelling, discomfort during bowel movements, or even bleeding in more severe cases. You might be surprised, but something as simple as persistent coughing can increase pressure in the lower abdomen—leading some to wonder, can coughing cause a hemorrhoid? While not a direct cause, it can indeed be a contributing factor.
Most hemorrhoids develop due to a combination of causes: chronic straining during bowel movements, constipation, prolonged sitting, or a low-fiber diet. Pregnancy and aging also increase the risk, as does a sedentary lifestyle. If you’ve ever dealt with the sharp discomfort of a stage 1 hemorrhoid, you know how quickly a minor irritation can escalate.
The good news? Your diet can make a big difference—both in relieving symptoms during a hemorrhoid flare-up and in preventing future problems. In fact, what you eat daily affects your stool consistency, bowel movement regularity, and the level of rectal inflammation your body experiences.
This article will guide you through everything you need to know about following a hemorrhoid diet—from what to eat and drink for fast relief, to herbal remedies and supplements that support gut health. Whether you’re currently struggling with painful symptoms or just trying to prevent future flare-ups, this guide is for you.
Why Diet Matters for Hemorrhoids
Diet is one of the most powerful and natural tools you can use to manage hemorrhoids. Whether you’re dealing with an active flare-up or trying to avoid future issues, what you eat directly affects your digestive system’s performance—especially your stool consistency and how easily you pass it.
How Diet Affects Stool Consistency
Hard, dry stools are one of the main culprits behind hemorrhoid pain and development. They require more straining to pass, which increases pressure on the rectal veins and can worsen inflammation. On the other hand, a soft, bulky stool moves more smoothly through the colon, reducing the need to push and strain.
This is why diets rich in fiber and water are recommended. Fiber adds bulk to the stool and helps it retain moisture, making bowel movements easier and more regular. This is crucial for preventing irritation, tears, and the cycle of swelling that defines hemorrhoid flare-ups.
Connection Between Fiber, Hydration, and Bowel Health
Fiber works best when paired with adequate hydration. Without enough fluids, fiber can actually make constipation worse. That’s why drinking plenty of water and including hydrating foods—like cucumbers and watermelon—alongside high-fiber meals is so important.
Hydration helps soften stools and supports smoother digestion, which in turn reduces the risk of aggravating both internal and external hemorrhoids. Dehydration, on the other hand, makes everything sluggish, increasing the chances of constipation and rectal strain.
Importance of Anti-Inflammatory Foods
Hemorrhoids involve swelling and irritation of the blood vessels around the anus. So naturally, adding anti-inflammatory foods into your daily diet can help reduce rectal inflammation and speed up healing. These include foods rich in antioxidants, flavonoids, and plant-based compounds that soothe the digestive tract.
Think of it as a double benefit: fiber keeps things moving, while anti-inflammatory ingredients calm the irritation. This approach not only addresses symptoms but also supports your gut health long-term.
And for those dealing with hemorrhoids during pregnancy, the question often comes up: how to get rid of a hemorrhoid while pregnant—diet is a gentle and safe place to start. Certain foods and natural remedies can offer relief without harsh side effects.
Best Foods for Hemorrhoids Relief and Prevention
A nourishing, gut-friendly diet can significantly reduce hemorrhoid symptoms and lower the chances of recurrence. Here are the most effective food categories to focus on, especially during a hemorrhoid flare-up.
High-Fiber Foods
Fiber is the foundation of a hemorrhoid-friendly diet. It softens stools, adds bulk, and promotes regular bowel movements—reducing strain and preventing further irritation.
- Whole grains like oats, brown rice, and barley are excellent staples. Oatmeal, for example, is a gentle option that can soothe the gut while providing soluble fiber.
- Fruits such as bananas, apples (with skin), pears, and especially papaya are helpful. Papaya contains enzymes that support digestion, making it a favorite in traditional diets for easing constipation.
- Vegetables like broccoli, spinach, carrots, and sweet potatoes offer both fiber and antioxidants.
- Legumes including lentils, chickpeas, and black beans help regulate bowel movements and support gut health.
Introducing these foods gradually helps avoid gas or bloating. Also, don’t forget to drink plenty of water to help fiber do its job effectively.
Foods Rich in Flavonoids
Flavonoids are natural compounds found in colorful plant foods. They’re known to strengthen blood vessel walls and reduce vascular inflammation, which is particularly useful for hemorrhoid healing.
- Berries, especially blueberries and blackberries
- Citrus fruits, including oranges and lemons
- Red cabbage, which is rich in anthocyanins
Eating these foods regularly may support the repair of swollen veins and promote faster recovery. In some cases, people notice relief from stage 1 hemorrhoid symptoms simply by improving circulation and reducing inflammation through flavonoid-rich meals.
Hydrating Foods and Fluids
Hydration plays a critical role in keeping stools soft and preventing constipation. In addition to drinking water, consuming water-rich foods enhances your hydration naturally.
- Cucumber, watermelon, and celery are great hydrating snacks.
- Herbal teas such as chamomile, peppermint, or ginger not only soothe the digestive tract but also count toward your fluid intake.
Dehydration is a sneaky trigger. It can turn a minor digestive slowdown into a painful bowel movement. In some cases, people find themselves wondering, can I pop a hemorrhoid? out of desperation—something that should definitely be avoided. Better hydration can help prevent that level of discomfort altogether.
Herbal & Natural Digestive Aids
Certain herbs and natural ingredients have been used traditionally to aid digestion, reduce inflammation, and support the body during a hemorrhoid flare-up.
- Papaya enzyme (papain) helps break down proteins and ease digestion.
- Psyllium husk is a gentle bulking agent and natural fiber supplement that promotes smoother bowel movements. It works especially well when taken with water before bedtime.
- Turmeric has strong anti-inflammatory effects and can be added to soups or smoothies.
- Red fruit oil (Buah Merah) is a Papua-grown herbal product rich in antioxidants and carotenoids. It’s traditionally used to support inflammation reduction and tissue repair.
- Aloe vera juice, in moderation, may soothe the digestive tract.
- Licorice root and slippery elm are calming herbs that help coat the intestinal lining, offering comfort during flare-ups.
Foods and Drinks to Avoid
Just as certain foods can support healing, others may trigger irritation, constipation, or flare-ups. Knowing what to avoid is just as important as knowing what to eat—especially if you’re actively dealing with symptoms.
Constipating Foods
These are foods that slow down digestion and lead to harder, more difficult-to-pass stools—one of the main triggers for hemorrhoid pain.
- Processed snacks such as chips, crackers, and cookies often lack fiber and are loaded with preservatives.
- White bread and other refined grains offer little nutritional value and can contribute to sluggish digestion.
- Cheese and other full-fat dairy products tend to be binding and can worsen constipation, especially if eaten in excess.
- Red meat, while not harmful in moderation, is harder to digest and lacks fiber. Eating too much can slow bowel movement regularity.
If you’re already dealing with bleeding or swollen hemorrhoids, avoiding these foods may help reduce pressure and discomfort.
Irritants to the Digestive Tract
Certain ingredients are known to irritate the gut lining or increase inflammation, both of which can worsen hemorrhoid symptoms.
- Spicy foods—including excessive chili, pepper flakes, or hot sauces—are a common trigger. Many people ask, can spicy food cause hemorrhoids? While it may not directly cause them, spicy meals can certainly aggravate existing ones.
- Caffeine, especially from coffee and energy drinks, can lead to dehydration and stimulate the gut in ways that disrupt regularity. The concern around coffee and hemorrhoids often relates to these effects.
- Alcohol dehydrates the body and may impair liver function, which can indirectly increase pressure in the lower veins.
Reducing or eliminating these items during a flare-up may provide faster relief and help prevent irritation from getting worse.
Low-Fiber Junk Foods
These are foods that offer empty calories and little to no fiber, making them the opposite of what your gut needs during hemorrhoid recovery.
- Fast food, with its high salt and fat content, slows digestion and often displaces more nutritious options.
- Fried snacks, including chips and deep-fried foods, are hard on the gut and contribute to inflammation.
- Refined sugar products, such as candies, pastries, and sweetened cereals, feed unhealthy gut bacteria and may worsen constipation.
Cutting back on these foods not only supports immediate symptom relief but also benefits your long-term gut health.
Sample 1-Day Hemorrhoid Diet Plan
If you’re unsure how to put all these food recommendations into practice, here’s a simple, balanced one-day meal plan designed to soothe hemorrhoid symptoms and support healing. It’s rich in fiber, hydration, and natural anti-inflammatory ingredients, while avoiding common triggers.
Breakfast
Oatmeal cooked with water or plant-based milk
Topped with banana slices, chia seeds, and a sprinkle of cinnamon
Cup of warm herbal tea (peppermint or chamomile)
This fiber-rich start helps keep bowel movements soft and regular, while soothing herbs relax the digestive system. Bananas are especially gentle, making them a great choice during a hemorrhoid flare-up.
Lunch
Brown rice with grilled chicken and steamed broccoli
Side of papaya slices
This meal offers a good mix of fiber, lean protein, and enzymes from papaya to support digestion. The broccoli provides both fiber and anti-inflammatory compounds.
Snack
A handful of prunes or raw almonds
Optional: small bowl of mixed berries for an antioxidant boost
Prunes are natural stool softeners thanks to their sorbitol content, which can be helpful if you’re dealing with irregularity or recovery from a stage 1 hemorrhoid.
Dinner
Lentil soup made with carrots, celery, and herbs
Side of whole-grain bread
Steamed spinach and carrots
This soothing, warm meal is high in fiber, iron, and antioxidants. The warmth can help relax the digestive system, similar to the benefits of a warm sitz bath.
Before Bed
1 teaspoon of psyllium husk stirred into a glass of warm water
Optional: cup of chamomile tea
Taken at night, psyllium husk works gently overnight to bulk and soften the stool for a more comfortable bowel movement the next morning.

Supplements and Herbal Products That May Help
While food is the foundation of a hemorrhoid-friendly lifestyle, certain supplements and herbal products like myrmecodia can offer added support—especially during flare-ups or if your daily routine makes it hard to get enough fiber naturally.
Fiber Supplements (Psyllium Husk)
Psyllium husk is a widely used natural fiber supplement that helps maintain stool bulk and softness. It acts as a gentle stool regulator, especially helpful for those with inconsistent fiber intake or sensitive digestion.
You can stir it into water or juice before bedtime—just be sure to follow with enough water to avoid the risk of further constipation. Regular use supports bowel movement regularity and prevents the kind of straining that can lead people to wonder, can I pop a hemorrhoid? (Short answer: no, and you shouldn’t try.)
Herbal Teas
Several herbal teas can help soothe the digestive tract and support better elimination:
- Peppermint tea helps reduce bloating and cramping.
- Chamomile tea calms the gut and supports relaxation.
- Ginger tea aids in digestion and may reduce mild inflammation.
These teas also help keep you hydrated—key for fiber to work effectively.
Magnesium Citrate
A natural stool softener, magnesium citrate draws water into the colon, making stools easier to pass. It can be taken occasionally during times of constipation or flare-up but should be used under guidance if taken long-term.
This gentle support may be especially useful for pregnant women wondering how to get rid of a hemorrhoid while pregnant, as magnesium is often included in prenatal supplements and is considered relatively safe in moderate doses.
Lifestyle Tips to Support the Diet
Even the best hemorrhoid diet works better when paired with healthy lifestyle habits. These small, consistent changes can make a big difference in preventing flare-ups and supporting long-term gut health.
Regular Bathroom Schedule
Try to go to the bathroom at the same time each day, ideally after meals. This helps train your digestive system to empty regularly. Don’t delay the urge to go—waiting too long can make stool harder and increase strain.
Avoid Straining
Straining is one of the biggest triggers for hemorrhoid development and pain. If bowel movements are difficult, pause, relax, and come back later rather than forcing it. Straining not only worsens symptoms but can also cause small tears or worsen inflammation. That’s partly why some people end up asking can coughing cause a hemorrhoid—since any increased abdominal pressure can contribute.
Light Exercise
Gentle movement helps stimulate digestion and improve blood flow to the lower body. Walking is especially beneficial and easy to incorporate into daily life. Avoid long periods of sitting—especially on hard surfaces—and try to stretch or move every hour if you have a desk job.
Sitz Bath
A warm sitz bath (sitting in a shallow basin of warm water) for 10–15 minutes can provide relief during active flare-ups. It helps relax the anal muscles, soothe irritation, and promote healing. This is often recommended during the recovery phase from bleeding or inflamed hemorrhoids.
Use a Footstool or Squatty Potty
Raising your feet while on the toilet (using a small stool or a specialized device) helps simulate a squatting position. This aligns the rectum more naturally, making bowel movements easier and reducing the need to strain. It’s a small shift that can bring major comfort, especially during flare-ups.
FAQs on Hemorrhoid Diet
Can spicy food cause hemorrhoids?
Spicy food doesn’t directly cause hemorrhoids, but it can certainly worsen symptoms. For those already dealing with a flare-up, chili, pepper sauces, or heavily spiced dishes may irritate the digestive tract and intensify the burning sensation during bowel movements. If you’re sensitive, it’s best to avoid them until symptoms subside.
Is coffee bad for hemorrhoids?
Coffee is a mixed bag. On one hand, it stimulates digestion and can promote bowel movements. On the other, it’s a diuretic and may lead to dehydration, which in turn can harden stools and increase the risk of straining. If you’re drinking coffee, make sure to hydrate well throughout the day to maintain stool softness and support gut health.
Can I eat meat with hemorrhoids?
Yes, but moderation is key. Lean meats like grilled chicken or fish are fine, especially when paired with fiber-rich vegetables and whole grains. However, red meat is harder to digest and lacks fiber, so it should be limited during a hemorrhoid flare-up. Overeating meat-heavy meals without enough fiber can make constipation worse.
Does fasting help hemorrhoids?
Fasting may temporarily reduce the frequency of bowel movements, which could bring relief during a painful flare-up. However, long-term fasting or skipping meals may backfire by slowing digestion and disrupting bowel regularity. If you try intermittent fasting, it’s important to eat fiber-rich, hydrating foods during your eating window.
Should I go vegan or vegetarian to prevent hemorrhoids?
A well-planned plant-based diet can be very effective for hemorrhoid prevention because it’s naturally high in fiber and antioxidants. However, you don’t need to give up meat entirely to see benefits. Even small increases in plant foods—fruits, vegetables, legumes, and whole grains—can support digestion and reduce flare-ups. It’s more about overall balance than strict dietary labels.
Conclusion
Hemorrhoids may be a common condition, but they don’t have to control your life. With the right diet, you can ease current symptoms and reduce the chances of flare-ups in the future. By focusing on fiber-rich foods, staying well-hydrated, and avoiding common dietary irritants, you’re giving your digestive system the support it needs to function smoothly.
Add in some gentle lifestyle habits—like walking daily, using a sitz bath, and avoiding strain—and you’re on your way to long-term relief. Herbal remedies and supplements like psyllium husk, magnesium citrate, or even traditional supports like herbal ant nest plant can complement these efforts when used thoughtfully.
Whether you’re dealing with a stage 1 hemorrhoid, managing symptoms during pregnancy, or simply trying to prevent future discomfort, these small, steady changes can make a big difference. And no matter how uncomfortable things may get, resist the urge to take extreme measures—yes, even if you’re wondering can I pop a hemorrhoid, the answer is always no.
Feel free to browse our herbal wellness products to find what suits your needs!